Avedon: Utilization Health Management Platform


“From the very beginning, Dev.Pro exceeded our expectations and quickly hired the developers we needed. The project tech stack required a specialist experienced in rather outdated technology and Dev.Pro was able to provide a Senior OpenEdge developer in just a few weeks.
We can recommend them as a 100% reliable software development partner.”

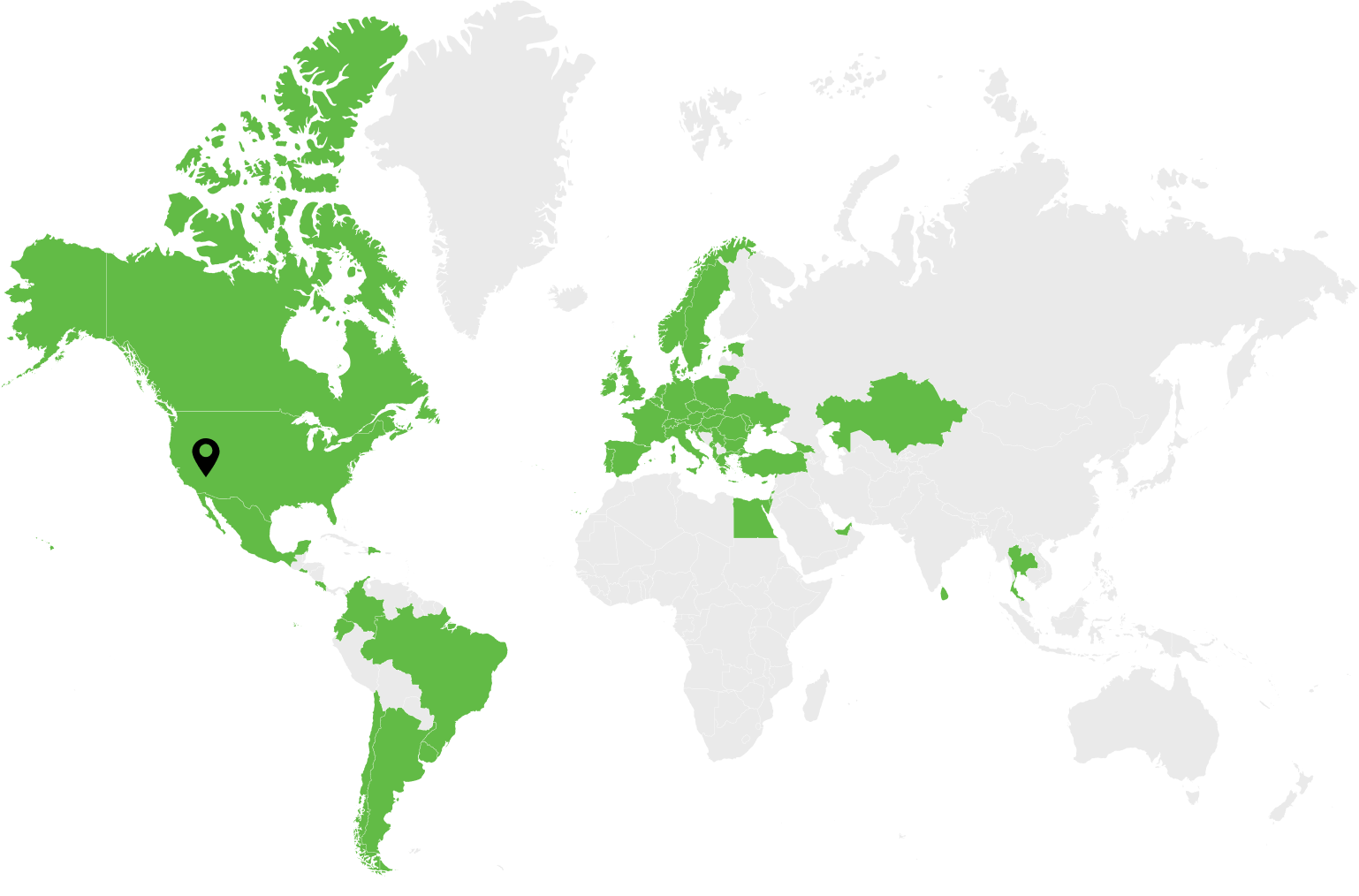
Payer Compass, part of Zelis, is a healthcare provider that offers market-leading healthcare cost containment services, price transparency, reference-based pricing, and more.
Zelis products help over 100 million members cut administrative costs, ensure payment integrity, and enable smooth payment processing while serving more than 700 payers and millions of providers.
Dev.Pro was involved in the continuous development of the AveCare management solution by Payer Compass, part of Zelis. AveCare is a disease management, patient advocacy, and utilization health management platform.
Our software engineers designed and developed features alongside data management, analytics and reporting technical requirements and objectives.
DEV.PRO CONTRIBUTION
Dev.Pro designed a mechanism for automatic report generation and distribution responsible for delivering 500+ daily, weekly, and monthly reports. This advanced automation feature led to a significant reduction in workload for the Operations Team of Payer Compass.
Dev.Pro helped create a tool for improving data quality that cleans up duplicated providers or insufficient information in line with strict Healthcare domain compliance frameworks.
The Dev.Pro team helped automate the data import process to allow eligibility data in different formats to be loaded automatically on the day of receipt, facilitating fast decision-making based on current information.
Dev.Pro helped to augment the Payer Compass team with a Senior OpenEdge developer who is now one of the team’s key project members.
TECHNOLOGIES
Contact us
Request to Speak with a Representative. Same-Day Consultations Available. Drop Us a Line.