Visium TM: Healthcare Claim Reimbursement Platform


“The Dev.Pro team quickly got up to speed on the project. They only needed 6 weeks to start performing as well as our in-house team.
Moreover, we’ve been impressed with their ability to find the right people quickly and augment the team with top-matched talents.
Thanks for our fruitful collaboration.”

Payer Compass, part of Zelis, is a healthcare provider that offers market-leading healthcare cost containment services, price transparency services, reference-based pricing, and more.
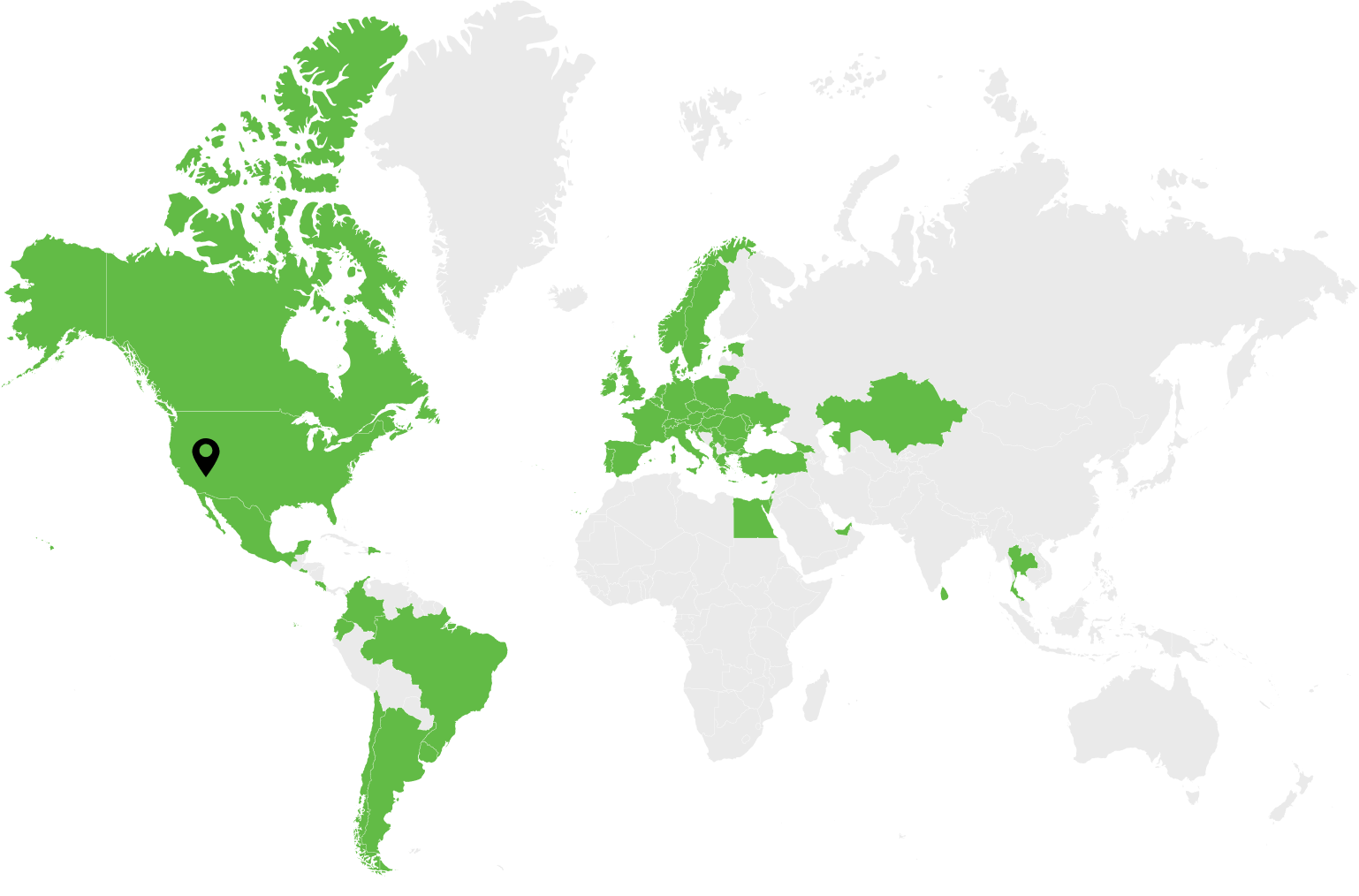
Zelis products help over 100 million members cut administrative costs, ensure payment integrity, and enable smooth payment processing while serving more than 700 payers and millions of providers.
Dev.Pro contributed to the development of a multi-faceted healthcare claim reimbursement platform called Visium TM by Payer Compass, part of Zelis.
This robust next-gen pricing transparency and contracting SaaS solution entails various features like health plan contract management, auditing and reporting, plan and claim modeling, and claim pricing and repricing tools. The tool allows processing of government contracts inclusive of Medicare and Medicaid.
DEV.PRO CONTRIBUTION
Dev.Pro helped form the backbone of a data loading team responsible for timely loads and adjustments to data.
Dev.Pro’s engineering team collaborated with Payer Compass to develop automatic data signalization, validation, and adjustment tools. The solution avoids SQL Server Integration Services package usage and decreases cycle time for each data loading request.
Dev.Pro participated in building customer and provider engagement portals from scratch. The end result helps eliminate complexities and paperwork, as well as increase transparency in healthcare pricing.
Dev.Pro helped integrate the product using RabbitMQ to provide uninterrupted data exchange with another client’s healthcare platforms.
TECHNOLOGIES
Contact us
Request to Speak with a Representative. Same-Day Consultations Available. Drop Us a Line.